If reading this article raises significant concerns for you, please reach out for help. Get in touch with your GP or if you are very distressed, please phone a helpline right now: Lifeline: 13 11 14 or the Butterfly National Help Line 1800 334673 which operates 8am-12 midnight, 7 days a week.
The last few years, with the pandemic and extended times of lockdown, has been a time of uncertainty, disappointment and isolation, providing a perfect storm for the development of eating disorders (EDs). It’s not only teenagers and young adults who are affected. In recent years, rates of EDs in boys and girls under 12 have been growing. This article is for parents facing this challenging and often lonely journey and aims to offer practical guidance for navigating an ED in your child or teen.
What’s up with my kid?
Olivia had taken ballet lessons for several years. Her chosen sport constantly drew attention to her body and her weight. As her body began to change and develop, Olivia was terrified of the natural increase in weight that came with growing up. Being a perfectionist, Olivia felt pressure from within to look just right. She started skipping meals to prevent her body from “getting fat.”
Cathy was worried about her ten-year-old daughter, Millie. After declaring herself a vegetarian a few months back, Millie was cutting out more and more foods, skipping breakfast before school and scrimping on other meals. While Millie had lost weight, she still looked healthy. Cathy had taken Millie to their family doctor. Her blood tests had all come back normal, but Cathy sensed something was not quite right with her daughter.
Camilla had begun to notice Sam, her son, wasn’t eating much. As a soccer player and a growing teen, shouldn’t he be eating her out of house and home? His lunchboxes were coming home untouched and he wasn’t eating much of anything at dinner. He was checking his body in the mirror a lot and had asked for a gym membership for his upcoming 14th birthday.
Mark was very alarmed at the marked change in his daughter’s behaviour since she had started online learning during the pandemic. Tilly often commented on how “fat and ugly” she looked on her screen’s camera, and spent hours in front of the mirror criticising her face and body. He tried to talk with her but she was moody, withdrawn and pushed him away.
Jacob was a strong swimmer who had recently started participating in competitions. He was weighed before training sessions and had been told he could do with losing some puppy fat. Embarrassed at this, he started regularly fasting before weigh-ins and then binged for days afterwards because of the intense hunger he felt after starving himself.
Olivia, Millie, Sam, Tilly and Jacob represent thousands of children and teenagers who are extremely concerned about their body image. Recent research has found that 50% of pre-adolescent girls (aged 8-11) and a similar number of boys are dissatisfied with their body. Approximately one third of Australian adolescents engage in disordered eating behaviours in any given year.
Have you observed changes in your child? Do you sense something is wrong with your teen? Or maybe you haven’t noticed anything unusual at all and wonder how you could have missed it? You are not alone. Eating disorders can emerge slowly and secretly, are often concealed and the signs can be subtle. In our diet-cultured world that adores thin and abhors fat, eating disordered behaviours are often deemed normal.
Some red flags may indicate a child or teenager is developing an ED:[1] These include:
- Unexplained changes in mood, grades, or friendships.
- Changes in food preferences, such as refusing previously enjoyed foods.
- Focus on appearance, body comparison or dissatisfaction followed by dieting or a desire to ‘get healthy’.
- Significant weight changes/fluctuations (even if they look healthy). Children and teens should be gaining weight quite predictably as they grow. Losing weight is not normal.
- Avoidance of family meals, insisting they are not hungry or have already eaten, or going to the bathroom following meals.
- Unusual behaviour around food, interest in food preparation and reading nutritional labels.
- Girls losing or experiencing disrupted periods.
- Missing food or food hidden in a bedroom, which is eaten secretly.
- Increased exercise.
- Tiredness, dizziness, coldness.
- Loss of interest in social activities.
Dieting is one of the strongest predictors for the development of an eating disorder. Weight loss and ‘fad’ diets do not take people’s individual requirements into consideration and can result in a person feeling hungry, experiencing low moods, lacking in energy levels and developing poor mental and physical health. The ‘diet cycle’ explains how many eating disorders can develop and are maintained. (See diagram below.)[2]

Eating Disorders in Children and Teenagers
EDs are brain-based illnesses that take over a person’s life and the lives of those closest to them. A number of factors can put a young person at higher risk of developing an ED, including:
- Existing mental health difficulties, such as anxiety.
- Personality traits, including being sensitive, a high achiever, having perfectionistic tendencies or low self-esteem.
- Stressful life events, such as divorce, bullying, abuse, onset of puberty, starting high school (or a global pandemic!)
- Challenges at school or within friendship groups.
- Pressures from the media to look a certain way, which children pick up from an early age.
- Involvement in sports where there is a focus on the body, such as gymnastics or swimming.
- Family history of eating disorders.
EDs are usually coping mechanisms for psychological stress. There are different types of EDs, each with its own features.[3] An ED can cause significant damage and disruption to a growing body. It also causes extreme emotional distress and a sense of separation from God.
Feelings are at the heart of eating disorders. Eating disorders can become a way to process feelings when we can’t talk about them with our loved ones. Learning to talk about feelings and emotions can be really helpful for children and teenagers, particularly if they are showing signs of developing an eating disorder. The diagram below might help provide a language scaffold for you to talk about feelings in the family. This diagram begins with ‘big’ feelings and then provides other words that apply to this emotion as well.[4]
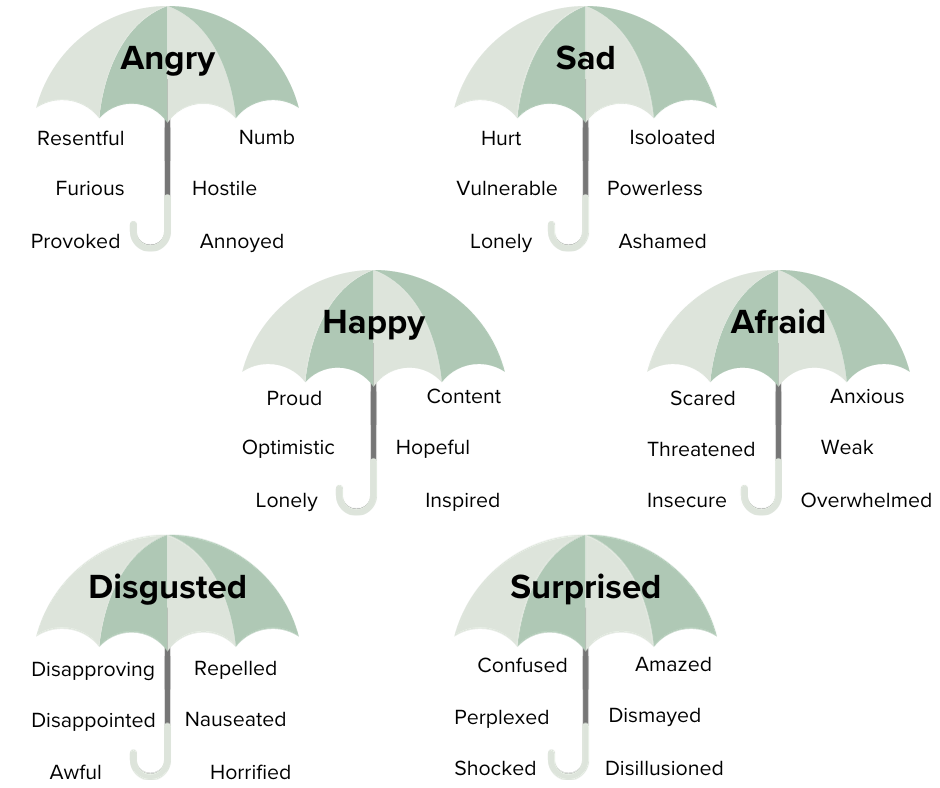
(from Ginny Jones Parent Coach – blog)
Treatment for Children and Adolescents
EDs require treatment to restore normal weight and eating habits, and to address the underlying psychological issues. The recommended evidence-based first-line treatment for children and adolescents is Maudsley Family Based Treatment (FBT).[5] This method acknowledges the importance of parents in a child’s life and empowers them to take control of their child’s eating at home, with three phases of treatment occurring. The treatment team teaches parents skills to support the recovery process. The family plays a crucial role and lasting recovery is possible.
FBT may not be appropriate or effective for every family. Other treatment options are available, including nutritional rehabilitation and psychological therapies.
What can you do to help your child?
To encourage healthy body image and a normal relationship with food, please never put your child on a diet, describe foods as “good” or “bad,” make negative comments about your own body or people in larger bodies, give your child body related compliments or praise weight loss.
If you suspect your child is showing signs of an ED, trust your instincts. Parents know their kids best. Remember it’s not your fault or your child’s fault. Living in a broken world means there will be illness, including for children. Early detection and prevention are key so it’s best to seek help, even if you think this could just be a phase.[6]
Equip yourself with knowledge about the illness.[7] It’s not recommended that teenagers be given information about EDs, as this often teaches them further disordered behaviours. Their job is to eat.
Remember this is an illness, so anger and tough love won’t work. Your child needs endless compassion and empathy. Listen to their concerns and remind them that you love them.
Anchor them in glorious biblical truths and pray these realities over them. Constantly remind them what our loving heavenly Father has to say about bodies and beauty in Genesis 1:27; Psalm 139:13-14; Proverbs 31:30, Ephesians 2:10 and 1 Peter 3:3-4. It can help to separate your child from the illness, seeing outbursts and lies as the ED not your child.
A good rule is life stops until you eat. This includes school, hobbies, social activities and phone/screen use. Privileges can be used as leverage for meal completion. Every meal will require supervision and meals can be long. Remain calm and firm.
Model healthy body image.[8] Find a Christian mentor to come alongside them. This doesn’t need to be someone who has recovered from an ED. They do need to be grounded in their own mature faith, have robust mental health and be a few years older. Mentors can be invaluable guides, encouraging your teen to fix their eyes on Jesus and reminding them that they don’t need to try harder, do more, look a certain way or prove their own worth because their Lord Jesus Christ has already done this.
It can be an overwhelming journey. A carer support group may help.[9]
Resources
- The Butterfly Foundation https://butterfly.org.au/
- Butterfly National Helpline https://butterfly.org.au/Get%20Support/Helpline/
More than 4000 parents or carers contact the National helpline each year – you are not alone.
- Eating Disorders Families Australia https://edfa.org.au/
- SupportWise (an online course for parents) https://www.supportwise.com.au/
When Your Teen Has an Eating Disorder: Practical Strategies to Help Your Teen Recover from Anorexia, Bulimia & Binge Eating book by Lauren Muhlheim
[1] A helpful checklist if you are concerned about your child http://feedyourinstinct.com.au/checklist/
[2] National Eating Disorders Collaboration https://nedc.com.au/
[3]You can read my earlier article that provides a summary of some of the different types of eating disorders. The Butterfly Foundation helpfully explains these different types as well. See https://butterfly.org.au/eating-disorders/eating-disorders-explained/
[4] The Ginny Jones Parent Coach Eating Disorders Blog provides some helpful tips here. https://ginnyjonescoach.com/eating-disorders-blog/
[5] A useful fact sheet about Family Based Therapy (FBT) https://www.eatingdisorders.org.au/wp-content/uploads/2019/04/EDV-Family-Based-Treatment.pdf
[6] Butterfly’s Referral Database can link you in with services near where you live https://butterfly.org.au/get-support/butterflys-referral-database/
[7] The Butterfly Foundation runs parent seminars to equip parents with information and tips https://butterfly.org.au/school-youth-professionals/for-schools/parent-seminars/
[8] Some helpful blogs for parents to assist with this:
- https://butterfly.org.au/body-image/modelling-healthy-body-image/
- https://butterfly.org.au/reducing-body-dissatisfaction-amongst-teens-how-parents-can-help/
- https://butterfly.org.au/back-to-school-a-body-image-and-mental-health-guide-for-parents-and-children/
[9] Butterfly offers carer support groups https://butterfly.org.au/get-support/face-to-face-support-groups/carersupportgroups/
Polly Manning holds a Bachelor of Education and taught in primary schools for a number of years. She has recently completed a Certificate of Pastoral Care followed by a Diploma of Christian Studies and is currently working through a Postgraduate Certificate of Pastoral Care for Mental Health. Polly is passionate about education, advocacy, and prevention of mental ill-health for children and adults. She has trained her dog, Henry, to work alongside her as an assistance dog. For fun, Polly enjoys gardening, reading, home decorating and cooking. She also loves serving across various ministries at her church.




